In healthcare, planning happens every day – often behind the scenes, yet it affects everything. Who uses which room, when nurses and doctors are available, and how schedules align with patient flow? These decisions shape how smoothly daily operations run and how effectively an organization’s spaces and resources actually serve patients.
Still, planning methods vary widely. In many units, calendars live separate lives in Excel sheets, emails, or sticky notes. Rooms are booked locally, schedules adjusted on the fly, and information flows best when a colleague happens to be in the break room. This is a classic example of decentralized planning – a model where each unit makes decisions independently.
But is this the most effective way to manage a complex system?
Local control brings flexibility and staff engagement
Decentralized planning is built on trust: departments and units know best what they need. Responsibility stays close to everyday operations, and the approach is often seen as fair and agile.
One of its biggest advantages is autonomy and the ability to react quickly. When schedules and room bookings are handled on-site, changes can be made immediately without managerial approval or long decision chains. For example, if a nurse calls in sick or an appointment is canceled, the unit can rearrange the day without delay.
Another strength is the ability to account for local needs. Each department has its own routines, patient groups, and equipment – such as physiotherapy rooms or specific diagnostic devices that aren't easily relocated. Local planning ensures these details are understood and taken into account.
The decentralized model is also easy to start with. It doesn't require major system investments, and existing tools can be used right away. For many organizations, this makes it a practical choice when resources are limited: Excel is quick, familiar, and doesn't require months of onboarding.
All in all, decentralized planning can work well in organizations where units operate independently and decisions are meant to stay close to frontline work.
When the big picture is missing, efficiency declines
Local flexibility is valuable – but it often comes at a cost when the broader picture is lost. Decentralized models may work well at the team level, but can lead to inefficiencies across the organization.
One of the main challenges is siloed work and underutilized resources. When each department optimizes only for itself, it's easy to end up with rooms and equipment standing idle in one unit while another struggles to meet demand. This is often visible in health centers: consultation rooms may go unused while a neighboring unit faces space shortages.
Another challenge is manual work and the potential for human error. Without a centralized system, planning is often done manually, which takes time. In some units, an administrator still updates door signs every morning to show who's using each room. When schedules change, the signage may not be updated, or a room booking might be missed entirely. These small errors add up, leading to delays and confusion for patients.
A third challenge is communication and transparency. When planning is scattered, leadership and other departments lack a clear overview. A staff member might be double-booked in two places at once, or patient flow may slow down because room information isn't updated in real time. This fragmentation causes stress at all levels, and no one has a clear picture of what's happening.
Additionally, decentralized models make system integration harder. If each unit has its own booking and planning processes, data can't easily be transferred to patient information systems, digital signage, or shared calendars. This leads to duplicate data, inconsistencies, and more administrative work.
Why is decentralized planning still so common?
It's easy to ask why this model is still used if its challenges are so well known. The answer often lies in history and habit. Decentralized planning has been the standard for decades. It has grown alongside organizations, and to many professionals, it feels familiar and manageable.
In many cases, centralized planning hasn't felt like a realistic option. System investments seemed too costly or complex, and local solutions felt quicker and easier.
So decentralized planning isn't inherently "wrong" – for a long time, it was the best available approach with the tools at hand. But as technology has evolved, the line between centralized and decentralized planning is starting to blur.
Moving toward shared visibility
Today, with tighter resources and increasing pressure to optimize space utilization, more organizations are turning toward centralized planning. Many are now asking:
"How can we gain a full view of the entire facility – without taking away local decision-making?"
This is the driving force behind many modern planning solutions that combine centralized visibility with local flexibility. These systems allow departments to continue making their own decisions while ensuring that information is accessible to everyone and that scheduling conflicts are automatically avoided.
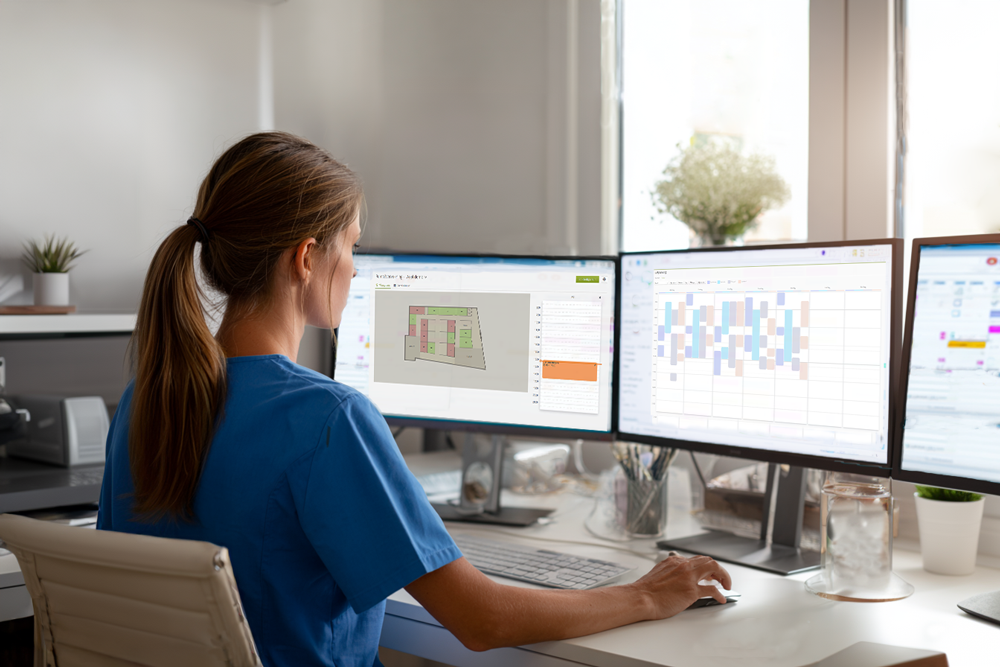
For example, Axel Planner was designed specifically to meet this need: it brings spaces, staff, and schedules together in one system, while allowing units to fine-tune their own planning. The result is greater transparency without added administrative burden – and the impact is visible in patient care.
Summary: Flexibility is good, but visibility is essential
Decentralized planning is a familiar and understandable model. It offers freedom and keeps decision-making close to day-to-day operations. But as organizations grow and resources tighten, local optimization alone isn't enough.
Without shared visibility and real-time information, inefficiency increases and duplicate work becomes unavoidable. That's why, in our next blog post, we'll look ahead: how centralized planning can combine efficiency with a human touch and allow professionals to focus on what matters most – the patient.
Next in the series: "Centralized planning – efficiency, transparency, and less manual work"